Cervical Fusion Surgery
Fusion of the Neck Vertebrae
By Jonathan Cluett, M.D., About.com Guide
Updated September 20, 2011
About.com Health's Disease and Condition content is reviewed by the Medical Review Board
See More About:
File for SSI DisabilitySocialSecurityLawFirms.com/FormHelpFind Out If You Qualify For Social Security Benefits. Free Evaluation!
Cervical Spinal Stenosiswww.SafeSpineSurgery.comTrust The Neuro-Ortho Specialists Best Of NYC Dr's Stern and Neubardt
A "cervical fusion" is the name for a surgical procedure that links together damaged segments of the vertebral column in the neck. This surgery is usually required when the cervical vertebrae -- and the discs between each vertebrae -- have become damaged as a result of an injury or chronic wear-and-tear. During surgery, the disc(s) between one or more vertebrae are removed, and bone growth is stimulated to link together adjacent vertebrae. Often, a metal device is used to stabilize the fusion until the bone growth is solid.
Cervical Fusion Surgery
A cervical fusion, also called an arthrodesis, permanently links together two (or more) adjacent vertebrae. Normally, there is a spinal disc between each vertebrae. The disc acts as a cushion, but also allows some movement between each vertebrae. Most often a cervical fusion is performed because the spinal disc is causing problems by pushing on a nerve (called a disc herniation). This nerve pressure can cause irritation leading to symptoms of pain, tingling, and numbness in the neck and arms. When a cervical fusion is performed, the disc, or fragments of the disc are removed. The bones of the vertebrae are then permanently linked together. This linkage occurs both with bone graft (the permanent solution) and often a metal plate, screw, or rod (the temporary solution). The metal simply holds the vertebrae in position while bone permanently fuses the segments together. Once the bone has linked the two vertebrae together, the fusion is considered solid, and resumption of normal activities is allowed.Recovery From Cervical Fusion
Recovery from cervical fusion depends on a number of factors. As mentioned, the surgery is considered a success when the symptoms are improved, and the bone has healed across the fused vertebrae. This fusion process usually takes 2 to 3 months. The activity allowed during that time will depend on the strength of the fusion. In some patients with solid bone and strong metal fixation more activity may be allowed. On the other hand, individuals who have concerns about their ability to fuse the vertebrae, the recovery may be more cautious.Complications From Surgery
The most common complication from surgery is basically that it fails to relieve the persistent neck pain. Fortunately, these complications are not common, but can occur. Studies have found success rates between 80 to 90% with cervical fusion surgical treatment for radiculopathy (nerve pain). The other potential major complication of a cervical fusion is a lack of adequate bone growth between the adjacent vertebrae. This is called an incomplete fusion, and may require additional surgery. Bone may not grow adequately for a number of reasons, and doing things like avoiding smoking and not taking medications or drugs that are known to interfere with bone growth. Other factors (such as a person's natural bone strength) are difficult to change. Other complications of cervical fusion can include nerve injury, difficulty swallowing, infection, and bleeding. Many patients are concerned about injury to the spinal cord. Of all of the complications listed, this is probably the least common. The risk of spinal cord injury is a small fraction of a percent.Alternatives to Cervical Fusion
If a patient only has a small disc herniation, often just the disc fragment can be removed without requiring a fusion. But if a patient needs the full-blown surgery, there aren't too many alternatives -- yet. There are new surgical procedures in development for spinal disc problems that are designed to remove the damaged disc, but still allow for movement at the affected vertebrae. These alternatives include dynamic stabilization and spinal disc replacement. More commonly performed in the lumbar spine (lower back), these procedures may help maintain motion while also solving the disc problem.
POSTED BY ATTORNEY RENE G. GARCIA:
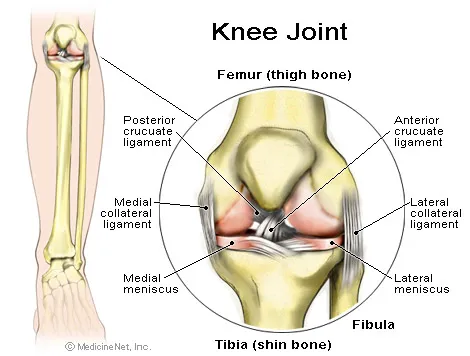
- Some of our clients have suffered major knee and leg injuries due to a serious accident. The Garcia Law Firm, P.C. was able to successfully handle these types of cases. For a free consultation please call us at 1-866- SCAFFOLD or 212-725-1313.
Link- http://orthopedics.about.com/od/spinalsurgery/qt/Cervical-Fusion-Surgery.htm
- Some of our clients have suffered major knee and leg injuries due to a serious accident. The Garcia Law Firm, P.C. was able to successfully handle these types of cases. For a free consultation please call us at 1-866- SCAFFOLD or 212-725-1313.
Link- http://orthopedics.about.com/od/spinalsurgery/qt/Cervical-Fusion-Surgery.htm




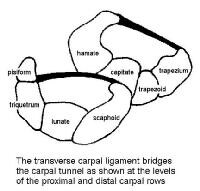

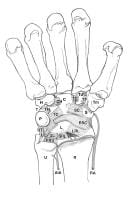
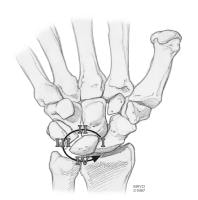
 If your hand is impaired in any way, surgery may improve your condition. This type of very specialized surgery can treat diseases that cause pain and impair the strength, function and flexibility of your wrist and fingers. Surgery seeks to restore to near normal the function of fingers and hands injured by trauma or to correct abnormalities that were present at birth. Specifically, hand surgery can treat:
If your hand is impaired in any way, surgery may improve your condition. This type of very specialized surgery can treat diseases that cause pain and impair the strength, function and flexibility of your wrist and fingers. Surgery seeks to restore to near normal the function of fingers and hands injured by trauma or to correct abnormalities that were present at birth. Specifically, hand surgery can treat:


